PLEASE SHARE THIS NEWSLETTER WITH YOUR RABIES PROGRAM TEAM AND ALL PUBLIC HEALTH INSPECTORS | |
|
What do you do when an animal is moved from one region to another prior to Request for Rabies Testing?
| |
Currently, the Request Submission Form includes the following question:
Was this animal imported into Ontario in the past 6 months?
The CFIA has requested that we also include if the animal has been moved from a different region than where the animal is being collected from. This will ensure that the CFIA takes this information into consideration in their analysis and that other jurisdictions are notified if the specimen returns as positive.
The most common example of the above situation is a wild animal that was moved to a wildlife rehabilitation centre that is located outside of the region the animal was found in.
The RRP is working with the software development team to add the regional question to the submission form. In the meantime, please include if the animal has moved from one region to the other, in the 10 days before exposure occurred, to the "Additional Notes" section at the bottom of the submission form.
| | | |
|
Risk Assessment Refresher
Written by: Dr. Maureen Anderson, Lead Veterinarian, Animal Health & Welfare, Veterinary Science Unit, OMAFRA
| |
We all know that a bite from a rabid animal that breaks the skin is a risk for rabies transmission. We are also all familiar with the plethora of scenarios that arise when it comes to potential rabies exposures that are not nearly so clean-cut! Taking some time to refresh our mindset about rabies transmission risks and discussing these scenarios with colleagues is important for helping us all use a consistent, risk-based approach to rabies response in Ontario.
Remember:
- Rabies can ONLY be transmitted from a LIVE animal through contact with SALIVA. There is no virus in blood, urine, feces or milk.
- High-risk tissues in a DEAD animal include brain, spinal cord, saliva / salivary glands.
- Saliva (or high-risk tissue) must come in contact with BROKEN skin or a mucous membrane (eyes, nose, mouth) – consider both bite and non-bite exposures, but scratches (from claws) alone are not a risk.
- Rabies is a very FRAGILE virus, that is inactivated very quickly in the environment (drying, heat, UV light, soap, etc.), but can be preserved by FREEZING
Risky: A person comes face-to-face with a hissing raccoon and gets saliva on their face.
Not risky: A person picks up a dead bat, and then washes their hands.
Not risky: A person comes in contact with blood from a skunk while washing off their dog.
Risky: A newly adopted dog (less than six months ago) with no previous known medical or travel history nips its owner who was trying to take away a toy.
Not risky: A dog excitedly jumps up on a visitor and scratches the person’s legs, drawing some blood.
Not risky: An adult wakes up to their cat jumping on the bed because there is a bat flying around the ceiling. The bat is not seen in direct contact with the bed or the cat.
Indirect Transmission Risk
- A person who has been exposed to a rabid animal (e.g. bat, raccoon, dog) is NOT considered a risk to other people (even through kissing, which is very clear exposure to saliva!), unless / until that person goes on to develop clinical rabies.
- Likewise, a dog or cat that has been exposed to a rabid animal is NOT considered a risk to other people or animals (even through licking or other exposure to saliva) immediately after the exposure occurs. It takes days (more often weeks to months) for the rabies virus to reach a pet’s brain and then subsequently be found in its saliva after an exposure.
-
Indirect transmission of rabies to human is extremely rare, and has only been reported with broken skin contact with saliva from rabid canids in fresh bite wounds (1,2). It has never been reported from contact with saliva on an animal’s fur. Dried saliva on fur (e.g. from self grooming) is not a risk for rabies transmission.
Risky: A dog and raccoon are fighting and the owner tries to separate them. The owner ends up with cuts on their arm, and can’t be sure if they came from the teeth or claws of the dog or the raccoon.
Not risky: A dog gets into a fight with a raccoon. The raccoon runs off. Half an hour later the dog is playing with the kids and licks their hands and faces.*
Not risky: A cat kills a bat. Shortly thereafter the cat scratches its owner (and no saliva from the cat gets in the scratches).
*not a risk for rabies transmission from the raccoon, but still a risk for transmission of various bacteria from the dog’s mouth!
Pet Bites - To vs From
Bites FROM a pet
- If a dog or cat bites a person, it should be observed for clinical signs of rabies for 10 days to determine if the person needs to receive rPEP.
- During the 10 day observation period, it is important to avoid any elective / non-urgent procedures (including vaccinations) that could inadvertently cause clinical signs in the animal that could be mistaken for signs of rabies infection.
- Historically, animals were vaccinated with modified live rabies vaccines. In very rare instances the vaccine strains could actually cause rabies in pets, so rabies vaccination during the 10 day observation period was prohibited. Modern rabies vaccines for domestic animals (which are killed or vectored) have eliminated this risk, but as with any vaccine a small percentage of animals may still have adverse reactions to any vaccine, which could transiently alter their behaviour.
Bite TO a pet
- If a dog or cat is exposed to a rabid animal, do NOT place it under a 10 day observation period.
- The pet should be revaccinated as soon as possible (unless rabies can be ruled out through testing). Think of this as post-exposure prophylaxis for the pet.
- The pet is then either observed or confined for 45 days or up to 6 months, depending on the risk and previous vaccination status. Pet owners should contact their veterinarian for advice and guidelines in these cases.
Bite to AND from a pet
- If a dog or cat is exposed to a rabid animal AND has bitten a person in the last 10 days (sometimes both can happen during the same incident):
- The pet should still be revaccinated as soon as possible (unless rabies can be ruled out through testing) in order to minimize the risk the pet will develop rabies.
- The pet should also be observed for clinical signs of rabies for 10 days to determine if the person needs to receive rPEP.
- Exposure of the pet to a rabid animal immediately prior to biting a person does NOT increase the risk of rabies transmission and does NOT automatically warrant rPEP.
- There is no need to extend the observation period beyond 10 days because the animal received a rabies vaccine during this period.
- If the animal shows signs or illness or abnormal behaviour after vaccination, it should be assessed by a veterinarian to help differentiate a vaccine reaction or other cause from onset of rabies.
| |
|
Here we will target specific questions that we have been asked by Public Health Inspectors. Usually when 1 person asks, there are several out there who are wondering the same thing so we wanted to share the answers with everyone. Please email any questions you have to rrp@oavt.org. If we don't know the answer we will do everything we can to find it for you.
Question: Sometimes more people are exposed to an animal which needs to be tested, could save rabies post exposure treatment for 5-6 family members. Just wondering if the OAVT could submit such specimens as urgent for testing over Thursday, Friday and weekends.
Answer:
Under normal circumstances specimens do not ship on Fridays or weekends due to the CFIA laboratory hours of operation and Purolator's service schedule. However, the CFIA will provide weekend/holiday testing in emergency situations.
AN ANIMAL WILL ONLY BE CONSIDERED FOR RABIES TESTING ON A WEEKEND OR HOLIDAY IF ALL OF THE FOLLOWING CRITERIA ARE SATISFIED:
-
The animal is reasonably suspected of being rabid, based on a thorough investigation including consideration of the animal species involved, its behaviour at the time of the exposure, presentation of clinical signs consistent with rabies, geographical area, and for domestic animals, potential for previous contact with a rabid animal.
-
The person has suffered a WHO Category III exposure (i.e., single or multiple transdermal bites or scratches, licks on broken skin, contamination of mucous membrane with saliva).
-
There is a medical contraindication to receiving post-exposure prophylaxis.
- The attending physician or Medical Officer of Health provides the laboratory with the name and telephone number of a contact who is readily available to receive and act upon the result on the day of testing. The laboratory must be able to speak with an individual, test results will not be left on an answering machine.
How to request Holiday/Weekend testing:
- The PHU has ensured the case satisfies the four established criteria
-
If all of the criteria are satisfied the PHU will contact the ministry’s Public Health Veterinarian at: Heather.McClinchey@ontario.ca
- After consultation with the PHU, Dr. Heather McClinchey will contact the OAVT Rabies Response Program to co-ordinate the collection and shipping of the sample.
-
The PHU will need to complete/submit the “OAVT Rabies Specimen Collection Request Form” which can be found at https://oavt.ca.thentiacloud.net/webs/oavt/register/#/rabies/phu-human. The contact name and phone number provided for results, by the attending physician or Medical Officer of Health, must be included in the request.
-
Once received, the OAVT RRP will FAX or scan a completed page 4 from the CFIA’s guide to the CFIA laboratory. This must be completed and received by the CFIA no less than 15 minutes PRIOR to the close of business on Friday (or the day before a Holiday) to inform the CFIA of the sample submission. Please note: Testing can only occur if courier service can be arranged. Ottawa has Saturday courier service but no Sunday/Holiday service available. Lethbridge has no weekend or holiday courier service available.
- OAVT will complete the CFIA electronic submission form and shipping documentation and will arrange the RVT for collection and shipping.
- The CFIA will report results to the contact provided by the attending physician or Medical Officer of Health, Dr. Heather McClinchey and the OAVT RRP.
| | | |
|
CFIA Report on Rabies in Canada
| |
The Canadian Food Inspection Agency has a website with statistics on all rabies cases in Canada (including the MNRF cases reported below) dating back to 1988. They update their website on the 28th day of each month.
As of October 31st, 2023 there has been a total of 2118 animals submitted across the country, including 1272 which were submitted by Ontario. Of these cases, 112 were positive for rabies, including 56 that were from Ontario.
The rabies positive cases in Ontario are distributed among the following species:
Visit the CFIA website for more information on rabies in Canada.
| |
|
Rabies in Ontario - MNRF Report
| |
The MNRF is reporting on their results of wildlife testing (with no human/animal exposure), surveillance and bait drops. As of November 29th, 2023 the MNRF is reporting a total of 523 cases (485 expired and 38 active) of raccoon strain and 21 cases (21 expired) of fox strain rabies in Ontario since the outbreak began in December 2015.
In 2023, the MNRF has tested a total of 2,867 animals and distributed over 671 000 baits. Below are the 2023 positive rabies results as of November 29th:
The total number of raccoon strain cases since the outbreak began in 2015 are distributed among the following Public Health Units:
- Hamilton: 215 raccoons, 112 skunks, 1 fox, 2 cats
- Haldimand-Norfolk: 30 raccoons, 2 skunks, 1 llama
- Niagara: 47 raccoons, 52 skunks, 1 dog
- Brant: 26 raccoons, 2 skunks
- Halton: 17 raccoons, 9 skunks
- Waterloo: 2 skunks
The total number of fox strain cases since the outbreak began in 2015 are distributed among the following Public Health Units:
- Perth: 6 cows, 2 skunks
- Huron: 1 cow, 3 skunks
- Waterloo: 1 fox, 5 skunks
- Wellington-Dufferin-Guelph: 3 skunks
The last case of fox strain rabies was detected in 2018. No cases have been detected in 2019-2022.
| 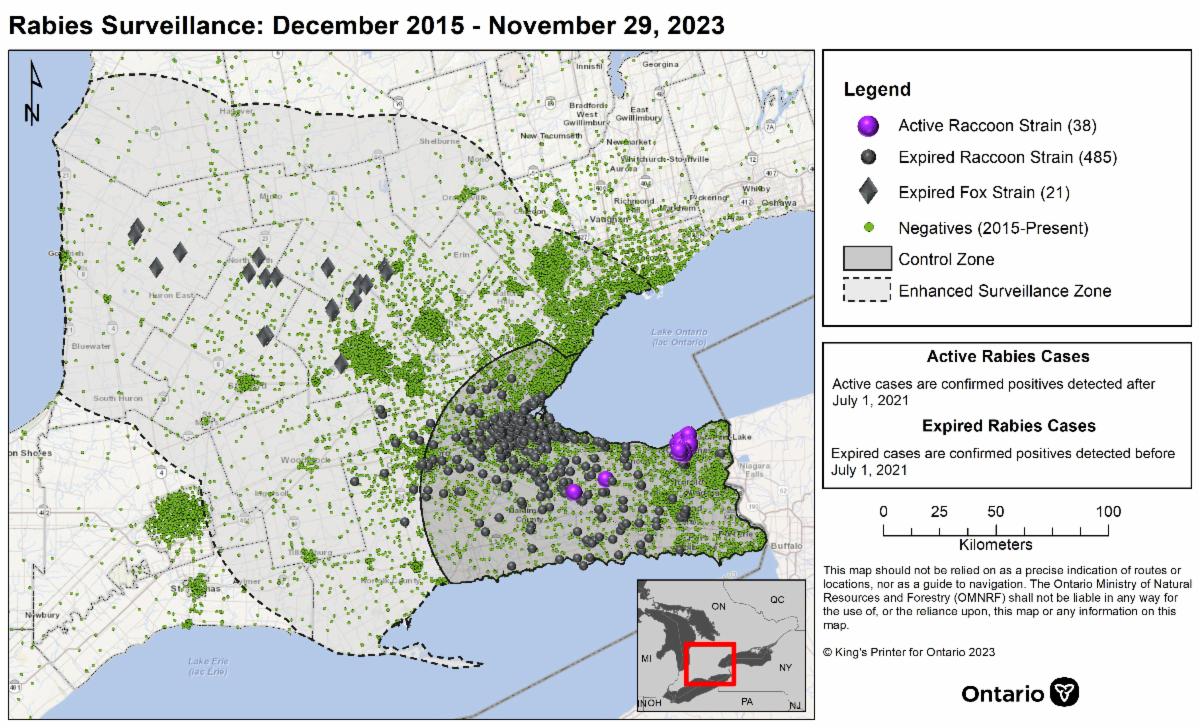 | The MNRF has launched a new interactive map to help provide more information about where rabies cases have been detected and where wildlife testing has been done. The map lets you select the testing year/s, strain types, and can be zoomed in to specific municipalities. | |
|
The OAVT Public Health Rabies Response Program Celebrates Their 10 Year Anniversary!
| |
On December 31, 2014 the RRP participated in their 1st collection and in their 10th year the program continues to thrive!
Since the program’s inception the OAVT RRP has worked with over 270 RVTs who have participated in over 11,800 collections while travelling over 729,000 kms helping to detect 219 positive rabies specimens, contributing to rabies surveillance in Ontario.
OAVT RRP Provincial Manager, Kristina Cooper and OAVT RRP Associate Manager, Tamara Gillen, both RVTs who initially created the functionality of the program from its inception and continue to lead the program, would like to extend their gratitude to both past and present RRP RVTs for participating in this important work. Kristina notes, “The unique skills of RVTs, their dedication to One Health in their communities along with their desire to provide excellent services to our Ministry of Health and Ontario Public Health Unit partners have been key to the success of the program.” Tamara mentions, “We are also grateful for the fantastic partnership we have shared with both the Ministry of Health and all of Ontario’s Public Health Units during the last decade who have supported the roles of RVTs in this capacity.”
| |
The OAVT Public Health Rabies Response Program
107-100 Stone Rd West
Guelph, ON
N1G 5L3
1-844-8RABIES
| | | | |