|
|

|
| I hope this newsletter finds you and your family well. I really enjoy fall weather. It always reminds me of high school and college cross-country season. There is nothing like running through the woods on a crisp fall day with leaves changing all around you. Hopefully, we will have several more days of mild temperatures so we can get out and enjoy the changing colors.
Last month, I highlighted a couple articles showing that exercise lowered risk of chronic diseases, including cancer. This month I have a couple articles that looks specifically at metabolic syndrome. This is several findings (high blood pressure, high triglycerides, high insulin levels) that lead to big problems. The first article looks at body fat and risk of cardiovascular disease. The study used CT scans to look both at the amount of fat and the types of fat. Guess what, fat is bad. Not a surprise, but the bigger point is that we can't just use body mass index (BMI) to evaluate risk for heart disease. New imaging may be a good way for use to check on our risk in the near future.
The second article continues in the metabolic syndrome vein. This study looked at overall survival for people with colorectal cancer. Avoiding or removing metabolic syndrome as a risk factor is important for survival if you are diagnosed with this cancer, but as we learned last month, the same things can help avoid getting the cancer in the first place.
My patients know I am a big proponent of vitamin D. The third study adds a compelling reason for people with asthma to add this supplement to their regimen. It just may keep you out of the hospital.
Click on the links the the left to check out our web site... |
|
Does This Scan Make Me Look Fat?
|
Amount and density of fat increases cardiovascular risk

We have all had our BMI calculated, perhaps at a doctor's appointment, by our employer's wellness screening, or maybe for an insurance physical. But is BMI a good way to calculate cardiovascular risk? Probably not. If often rates more muscular people as overweight or even obese and people in the optimum range may not be healthy. In fact, some studies have shown better health in people in the 'overweight' or 'mildly obese' categories. How about waist circumference to evaluate for risk? We know that men with waist measurements over 40 inches and women with measurements over 35 inches may be at higher risk. So this is better, right? Well, maybe, but it's still not optimum. This study, from the October edition of the
Journal of the American College of Cardiology questions all of this. This study collected data on 1,106 men and women with an average age of 45 over a 6-year period of time using abdominal adipose tissue imaging (CT scan) to evaluate both subcutaneous fat (beneath the skin) and visceral fat (around the internal organs) and found that more fat led to higher risk. Visceral fat is associated with insulin resistance, abnormal lipids, and fatty liver.
Abstract:
-
Background: Subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT) are associated with adverse cardiometabolic risk profiles.
-
Objectives: This study explored the degree to which changes in abdominal fat quantity and quality are associated with changes in cardiovascular disease (CVD) risk factors.
-
Methods: Study participants (n = 1,106; 44.1% women; mean baseline age 45.1 years) were drawn from the Framingham Heart Study Third Generation cohort who participated in the computed tomography (CT) substudy Exams 1 and 2. Participants were followed for 6.1 years on average. Abdominal adipose tissue volume in cm3 and attenuation in Hounsfield units (HU) were determined by CT-acquired abdominal scans.
-
Results: The mean fat volume change was an increase of 602 cm3 for SAT and an increase of 703 cm3 for VAT; the mean fat attenuation change was a decrease of 5.5 HU for SAT and an increase of 0.07 HU for VAT. An increase in fat volume and decrease in fat attenuation were associated with adverse changes in CVD risk factors. An additional 500 cm3 increase in fat volume was associated with incident hypertension (odds ratio [OR]: 1.21 for SAT; OR: 1.30 for VAT), hypertriglyceridemia (OR: 1.15 for SAT; OR: 1.56 for VAT), and metabolic syndrome (OR: 1.43 for SAT; OR: 1.82 for VAT; all p < 0.05). Similar trends were observed for each additional 5 HU decrease in abdominal adipose tissue attenuation. Most associations remained significant even after further accounting for body mass index change, waist circumference change, or respective abdominal adipose tissue volumes.
-
Conclusions: Increasing accumulation of fat quantity and decreasing fat attenuation are associated with worsening of CVD risk factors beyond the associations with generalized adiposity, central adiposity, or respective adipose tissue volumes.
This study is potentially a very important addition to the medical literature. It shows that we have a way to directly measure possible risk and also follow changes which would reduce risk. In this study, each pound of fat was associated with higher risk of metabolic syndrome (hypertension, high triglycerides, low HDL, impaired glucose tolerance) which is a known risk for cardiovascular disease. Rather than relying on imperfect measurements like BMI, we can now directly measure fat for more accurate measurements of risk. The other benefit is that we can look at the density of the fat. As fat becomes less dense, it becomes more metabolically active and thus more dangerous. These are newer techniques being worked on, but I am hopeful that they will soon be something that can easily and inexpensively be done.
Regardless of our ability to measure, this shows that less fat is better and we can definitely improve our risk profile with dietary changes and exercise (see last month's newsletter) which lowers our risk of
metabolic syndrome. We don't need a CT scan to know if we are carrying too much fat in most cases. How do we do this? A Mediterranean type diet (low sugar and starch) along with regular exercise.
|
Metabolic Syndrome Increases Mortality in Colrectal Cancer
|
Higher death rate in those with multiple risk factors
Colorectal cancer is the third most common cancer diagnosed in both men and women in the United States with around 135,000 new cases diagnosed and almost 50,000 deaths
annually. This death rate has been dropping due to more screening leading to earlier detection and treatment, but it is still significant. This study, from the
Journal of Clinical Oncology, set out to identify high-risk groups of patients and found that those with obesity and
metabolic syndrome had worse survival when diagnosed with colon cancer.
-
Purpose: The effects of obesity and metabolic dysregulation on cancer survival are inconsistent. To identify high-risk subgroups of obese patients and to examine the joint association of metabolic syndrome (MetSyn) in combination with obesity, we categorized patients with early-stage (I to III) colorectal cancer (CRC) into four metabolic categories defined by the presence of MetSyn and/or obesity and examined associations with survival.
-
Methods: We studied 2,446 patients diagnosed from 2006 to 2011 at Kaiser Permanente. We assumed MetSyn if patients had three or more of five components present at diagnosis: fasting glucose > 100 mg/dL or diabetes; elevated blood pressure (systolic ≥ 130 mm Hg, diastolic ≥ 85 mm Hg, or antihypertensives); HDL cholesterol < 40 mg/dL (men) or < 50 mg/dL (women); triglycerides ≥ 150 mg/dL or antilipids; and/or highest sex-specific quartile of visceral fat by computed tomography scan (in lieu of waist circumference). We then classified participants according to the presence (or absence) of MetSyn and obesity (BMI < 30 or ≥ 30 kg/m2) and assessed associations with overall and CRC-related survival using Cox proportional hazards models adjusted for demographic, tumor, and treatment factors and muscle mass at diagnosis.
-
Results: Over a median follow-up of 6 years, 601 patients died, 325 as a result of CRC. Mean (SD) age was 64 (11) years. Compared with the reference of nonobese patients without MetSyn (n = 1,225), for overall survival the hazard ratios (HR) and 95% CIs were 1.45 (1.12 to 1.82) for obese patients with MetSyn (n = 480); 1.09 (0.83 to 1.44) for the nonobese with MetSyn (n = 417), and 1.00 (0.80 to 1.26) for obese patients without MetSyn (n = 324). Obesity with MetSyn also predicted CRC-related survival: 1.49 (1.09 to 2.02). The hazard of death increased with the number of MetSyn components present, independent of obesity.
-
Conclusion: Patients with early-stage CRC with obesity and MetSyn have worse survival, overall and CRC related.
Th
is study shows that once again, the idea of metabolic syndrome is quite dangerous for our long-term health. Much of this likely relates to inflammation which is triggered by higher insulin levels due to insulin resistance. Again, the treatment is clear. If you want to have a better survival rate for colorectal cancer, avoid getting metabolic syndrome. Of course, last month I highlighted an article that also showed that exercise and a healthy diet lower the risk of even getting cancer. So let's prevent it before we even get it! That's the best result of all!
|
|
Sunshine Vitamin Helps with Asthma
|
Vitamin D shown to help prevent asthma attacks
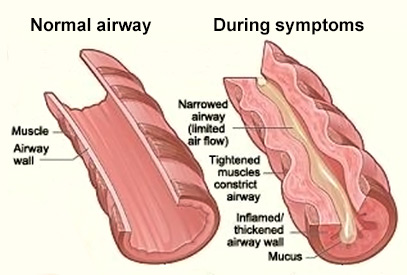
Asthma affects 24 million adults and children in the US and accounts for over 10 million office visits annually. Low levels of vitamin D have been linked to increased risk of asthma attacks. This study, from the
Cochrane Database of Systematic Reviews, looked at 7 trials with 435 children and 658 adults comparing vitamin D intake to placebo. They found that people given vitamin D had fewer asthma attacks needing hospitalization or treatment with oral steroids.
Abstract:
-
Background:
Several clinical trials of vitamin D to prevent asthma exacerbation and improve asthma control have been conducted in children and adults, but a meta-analysis restricted to double-blind, randomised, placebo-controlled trials of this intervention is lacking.
-
Objectives:
To evaluate the efficacy of administration of vitamin D and its hydroxylated metabolites in reducing the risk of severe asthma exacerbations (defined as those requiring treatment with systemic corticosteroids) and improving asthma symptom control.
-
Search methods:
We searched the Cochrane Airways Group Trial Register and reference lists of articles. We contacted the authors of studies in order to identify additional trials. Date of last search: January 2016.
-
Selection criteria:
Double-blind, randomised, placebo-controlled trials of vitamin D in children and adults with asthma evaluating exacerbation risk or asthma symptom control or both.
-
Data collection and analysis
Two review authors independently applied study inclusion criteria, extracted the data, and assessed risk of bias. We obtained missing data from the authors where possible. We reported results with 95% confidence intervals (CIs).
-
Main results:
We included seven trials involving a total of 435 children and two trials involving a total of 658 adults in the primary analysis. Of these, one trial involving 22 children and two trials involving 658 adults contributed to the analysis of the rate of exacerbations requiring systemic corticosteroids. Duration of trials ranged from four to 12 months, and the majority of participants had mild to moderate asthma. Administration of vitamin D reduced the rate of exacerbations requiring systemic corticosteroids (rate ratio 0.63, 95% CI 0.45 to 0.88; 680 participants; 3 studies; high-quality evidence), and decreased the risk of having at least one exacerbation requiring an emergency department visit or hospitalisation or both (odds ratio (OR) 0.39, 95% CI 0.19 to 0.78; number needed to treat for an additional beneficial outcome, 27; 963 participants; 7 studies; high-quality evidence). There was no effect of vitamin D on % predicted forced expiratory volume in one second (mean difference (MD) 0.48, 95% CI -0.93 to 1.89; 387 participants; 4 studies; high-quality evidence) or Asthma Control Test scores (MD -0.08, 95% CI -0.70 to 0.54; 713 participants; 3 studies; high-quality evidence). Administration of vitamin D did not influence the risk of serious adverse events (OR 1.01, 95% CI 0.54 to 1.89; 879 participants; 5 studies; moderate-quality evidence). One trial comparing low-dose versus high-dose vitamin D reported two episodes of hypercalciuria, one in each study arm. No other study reported any adverse event potentially attributable to administration of vitamin D. No participant in any included trial suffered a fatal asthma exacerbation. We did not perform a subgroup analysis to determine whether the effect of vitamin D on risk of severe exacerbation was modified by baseline vitamin D status, due to unavailability of suitably disaggregated data. We assessed two trials as being at high risk of bias in at least one domain; neither trial contributed data to the analysis of the outcomes reported above.
-
Authors' conclusions:
Meta-analysis of a modest number of trials in people with predominantly mild to moderate asthma suggests that vitamin D is likely to reduce both the risk of severe asthma exacerbation and healthcare use. It is as yet unclear whether these effects are confined to people with lower baseline vitamin D status; further research, including individual patient data meta-analysis of existing datasets, is needed to clarify this issue. Children and people with frequent severe asthma exacerbations were under-represented; additional primary trials are needed to establish whether vitamin D can reduce the risk of severe asthma exacerbation in these groups.
Asthma is a common affliction affecting approximately 8% of the population. This well-done review showed that vitamin D supplementation decreased the severity and fequency of asthma attacks required hospital visits or oral steroids. This is a cheap, easy, and safe way to decrease problems. The authors don't make a specific recommendation on dosage, but I usually recommend 2000-5000 IU daily in a capsule, liquid, or gel cap form.
|
|
Thank you for taking the time to read through this newsletter. I hope you have found this information useful as we work together to optimize your health.
It seems we are always finding more ways that a healthy diet and exercise program can help prevent or improve survival for one of the terrible afflictions that we can get. This month it's heart disease and colon cancer. Don't forget, these healthy habits help with even more diseases.
Once again, vitamin D is being shown to be of benefit. There are very few reasons not to take it, especially if you have asthma.
As always, if you have questions about anything in this newsletter or have topics you would like me to address, please feel free to contact me by email, phone, or just stop by!
To Your Good Health,
Mark Niedfeldt, M.D.
|
|
|