|
People say with certainty that no one has immunity to the SARS-CoV-2 virus, the virus that causes COVID-2019 disease. However, the one member of a cohabiting family who remains uninfected when all the others have fallen ill must have some immunity.
SARS-CoV-2 is the seventh known coronavirus, following SARS-CoV-1, MERS and four types that cause the common cold. What makes a virus family a family is that viruses in that family have commonalities different from those of other virus families. Those common features are their surface proteins that determine structure, host specificity, and virulence, as described in my last article (
Viral Virulence - Part 2) In the case of viruses, someone with immunity has antibodies to one or more of those surface proteins.
Our immune system has two attack mechanisms that are specific for fighting a given infection. In one type, cells contain or destroy foreign organism
 s, such as tuberculosis. The other employs circulating proteins (antibodies) that attach to and initiate processes that kill the invader. Against viruses, antibodies confer immunity, after both infection and vaccination.
s, such as tuberculosis. The other employs circulating proteins (antibodies) that attach to and initiate processes that kill the invader. Against viruses, antibodies confer immunity, after both infection and vaccination.
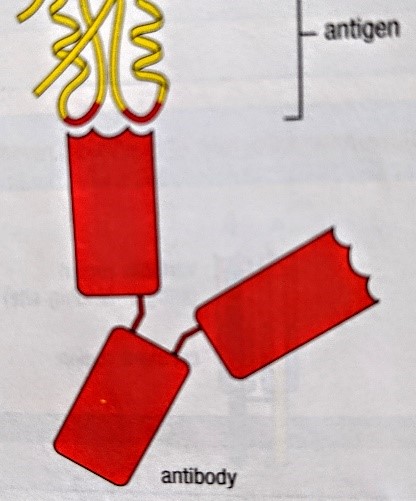
Antibodies are Y-shaped proteins that circulate in blood and confer immunity. The Y's upper arms specifically recognize and bind to small sections of proteins called antigens that the body thinks are foreign. The bottom tail of the antibody, of which there are 5 types, determines what the antibody does with the antigen after binding. Some antigens are more immunogenic than others, meaning they are more likely to be recognized as a bad foreign thing to be attacked.
When we fight off a viral infection, we likely make antibodies to more than one antigen on the virus' surface. Some of those antibodies may be completely ineffectual in stopping infection and others may stop the virus cold. Three factors ensure that the latter prevails: 1) The viral protein to which an antibody binds must be important to virulence; 2) the antibody binding must not be weak; and 3) the antibody type (the bottom of the Y) must be a type that efficiently initiates killing. It's like the difference between a lion chomping on your neck vs. a tiny dog latching onto a toe.
With SARS-CoV-2, scientists assume that the crucial surface protein is the spike protein which punctures our cells' surfaces, enabling viral entry. This protein is the focus of most vaccine research.
Back to pre-COVID-2019 coronavirus immunity - Scientists know that coronaviruses that cause the common cold induce antibody immunity that generally lasts about a year. Usually we don't know which virus has caused our cold. If it is a coronavirus, we don't know to which viral surface proteins recovering cold sufferers make antibodies. And we don't know if those antigens are present on SARS-CoV-2, and, if they are, how important they are to its virulence.
The bottom line is this: The fact that some people who should be ill with the virus are not suggests that there is some, at least partial, immunity in those people, likely derived from a prior cold caused by coronavirus.
To come: Virus vs. antibody testing and vaccines.
|