|
|

|
|
Welcome to the July newsletter. The goal of this newsletter is to provide information and analysis of timely topics from recent articles published in the medical literature. I hope you find this information useful and helpful in your health journey.
The end of July is always a bit bittersweet for me. We have plenty of summer weather left but it seems like it is slipping away so quickly. I never seem to make enough progress on my "to do this summer" list. There is always more I'd love to do outdoors while we have nice weather.
Cancer is the number two killer in the United States, not far behind number one, heart disease. It is one of the things we all worry about as we age. What can we do to prevent cancer deaths? What if I told you there was a free (!) intervention that could reduce cancer mortality by over 50%? What if there was a simple change you could make in your daily routine to get this benefit? If you are interested, check out the first article.
Staying on the topic of living longer (and better). What is the best type of exercise to increase lifespan and reduce mortality from all causes? Is is cardio or aerobic exercise? Is weight training the way to go? The second article looks at the specific types of exercise (and amounts) to give us guidance as we work on living better. As an added bonus, there is a tip for reducing mortality from a virus.
We are having passionate discussions on reopening schools. Children need to be in school. Can we do this in the face of a pandemic? Children can get COVID-19. How does it affect them? How much do they spread it? What is the economic impact of schools being closed? What will the long-term effects be on our children? I had this section all written when some breaking information came through. I'll give you a preview. It's complicated.
Information is constantly changing. If you are feeling sick or concerned about symptoms, please call me first. We can discuss your symptoms and decide the best course of action for you, including testing. I now have saliva based COVID-19 PCR tests available in my office with 24+ hour turnaround. Serum antibody tests can be performed as well with 24-hour turnaround. I am working on point of care testing and will hopefully have this in place when I write you next. Please continue to wash your hands frequently, avoid touching your face, and avoid going out if you are sick.
|
|
Sit More, Die More
|
Sedentary behavior associated with higher cancer mortality
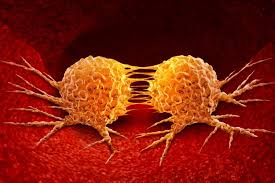
It is commonly known that physical activity reduces mortality from the number one killer in the U.S., heart disease. But what about the second biggest killer, cancer? This study from JAMA Oncology, used hip mounted accelerometers to measure physical activity in 8002 subjects and followed the group for a mean of 5.3 years. The group included 54% women and the mean age was 69.8 yrs. The subjects were categorized into three groups based on documented activity; sedentary, light intensity, and moderate to vigorous intensity physical activity. Over the follow up period 3.3% of the participants died of cancer. The researchers found that the most sedentary group was 45% more likely to die of cancer than the light intensity group, and 52% more likely to die than the most active group.
- IMPORTANCE: Sedentary behavior is associated with several health outcomes, including diabetes, cardiovascular disease, and all-cause mortality. Less is known about the association between objectively measured sedentary behavior and cancer mortality, as well as the association with physical activity.
- OBJECTIVE: To examine the association between accelerometer-measured sedentary behavior (total volume and accrual in prolonged, uninterrupted bouts) and cancer mortality.
- DESIGN, SETTING, AND PARTICIPANTS: A prospective cohort study conducted in the contiguous US included 8002 black and white adults aged 45 years or older enrolled in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. The present analysis was performed from April 18, 2019, to April 21, 2020.
- EXPOSURES: Sedentary time, light-intensity physical activity (LIPA), and moderate- to vigorous-intensity physical activity (MVPA) were measured using a hip-mounted accelerometer worn for 7 consecutive days.
- MAIN OUTCOMES AND MEASURES: Cancer mortality.
- RESULTS: Of the 8002 study participants, 3668 were men (45.8%); mean (SD) age was 69.8 (8.5) years. Over a mean (SD) follow-up of 5.3 (1.5) years, 268 participants (3.3%) died of cancer. In multivariable-adjusted models, including MVPA, greater total sedentary time was associated with a greater risk of cancer mortality (tertile 2 vs tertile 1: hazard ratio [HR], 1.45; 95% CI, 1.00-2.11; tertile 3 vs tertile 1: HR, 1.52; 95% CI, 1.01-2.27). Longer sedentary bout duration was not significantly associated with greater cancer mortality risk: after adjustment for MVPA (tertile 2 vs tertile 1: HR, 1.26; 95% CI, 0.90-1.78; tertile 3 vs tertile 1: HR, 1.36; 95% CI, 0.96-1.93). Replacing 30 minutes of sedentary time with LIPA was significantly associated with an 8% (per 30 minutes: HR, 0.92; 95% CI, 0.86-0.97) lower risk of cancer mortality; MVPA was significantly associated with a 31% (per 30 minutes: HR, 0.69; 95% CI, 0.48-0.97) lower risk of cancer mortality.
- CONCLUSIONS AND RELEVANCE: In this cohort study, greater sedentary time, as measured with accelerometry, appeared to be independently associated with cancer mortality risk. Replacing sedentary time with either LIPA or MVPA may be associated with a lower risk of cancer mortality. These findings suggest that the total volume of sedentary behavior is a potential cancer mortality risk factor and support the public health message that adults should sit less and move more to promote longevity.
The more you sit the more likely you will die of cancer. That is the take home message of this study. More time being sedentary was independently associated with increased cancer mortality. This study is unique as most studies use surveys to assess activity, while this one directly measured activity. The found that the more active subjects were, the lower their risk of cancer death with the difference between the sedentary group and the moderate to vigorous exercise group was 52%! Replacing 30 minutes of sedentary time with 30 minutes of light physical activity lowered risk by 8% and replacing with moderate to vigorous activity lowered risk by a whopping 31%! Additionally, there was a trend toward increased risk with prolonged sedentary sessions. It makes sense to break up sedentary periods with activity as much as possible. It will reduce your risk of dying of cancer and it's good for you heart and overall health!
|
|
|
What is the best exercise type to reduce all-cause mortality?
Physical inactivity is estimated to account for 9% of premature deaths and 45.9% of global healthcare costs. The 2018 physical activity guidelines for Americans, recommends that adults should engage in at least 150 minutes of moderate intensity aerobic physical activity or at least 75 minutes of vigorous intensity aerobic physical activity each week, or an equivalent combination of both. Furthermore, adults should engage in muscle strengthening activities of moderate or greater intensity on two days or more each week. Do the current recommendations and guidelines for physical activity really reduce mortality? What about mortality for specific conditions? This study sought to answer these specific questions. The authors evaluated the relationship of recommendations for physical activity and all-cause and cause-specific mortality in a group of almost 480,000 people. They evaluated the amount of time spent on physical activity as well as the type of physical activity, specifically aerobic activity, muscle-strengthening activity, or a combination of the two types and evaluated the relationship between these factors and all-cause and cause-specific mortality. The good news is that all types of activity reduced mortality. The greatest effect, a 40% reduction in mortality was found with a combination of aerobic and muscle strengthening activities.
Abstract:
- OBJECTIVE: To determine the association between recommended physical activity according to the 2018 physical activity guidelines for Americans and all cause and cause specific mortality using a nationally representative sample of US adults.
- DESIGN: Population based cohort study.
- SETTING: National Health Interview Survey (1997-2014) with linkage to the National Death Index records to 31 December 2015.
- PARTICIPANTS: 479,856 adults aged 18 years or older.
- EXPOSURES: Participant self-reports of the amount of leisure time spent in aerobic physical activity and muscle strengthening activity each week were combined and categorised into four groups: insufficient activity, aerobic activity only, muscle strengthening only, and both aerobic and muscle strengthening activities according to the physical activity guidelines.
- MAIN OUTCOME MEASURES: All cause mortality and cause specific mortality (cardiovascular disease, cancer, chronic lower respiratory tract diseases, accidents and injuries, Alzheimer's disease, diabetes mellitus, influenza and pneumonia, and nephritis, nephrotic syndrome, or nephrosis) obtained from the National Death Index records.
- RESULTS: During a median follow-up of 8.75 years, 59,819 adults died from all causes, 13,509 from cardiovascular disease, 14,375 from cancer, 3,188 from chronic lower respiratory tract diseases, 2,477 from accidents and injuries, 1,470 from Alzheimer's disease, 1,803 from diabetes mellitus,1,135 from influenza and pneumonia, and 1,129 from nephritis, nephrotic syndrome, or nephrosis. Compared with those who did not meet the physical activity guidelines (n=268,193), those who engaged in recommended muscle strengthening activity (n=21,428; hazard ratio 0.89, 95% confidence interval 0.85 to 0.94) or aerobic activity (n=113,851; 0.71, 0.69 to 0.72) were found to be at reduced risk of all cause mortality; and even larger survival benefits were found in those engaged in both activities (n=76,384; 0.60, 0.57 to 0.62). In addition, similar patterns were reported for cause specific mortality from cardiovascular disease, cancer, and chronic lower respiratory tract diseases.
- CONCLUSIONS: Adults who engage in leisure time aerobic and muscle strengthening activities at levels recommended by the 2018 physical activity guidelines for Americans show greatly reduced risk of all cause and cause specific mortality. These data suggest that the physical activity levels recommended in the guidelines are associated with important survival benefits.
We know that physical activity is good for us and is associated with lower risk of several chronic conditions. People often ask what is the best type of exercise to do? My standard answer is to do the one that you enjoy and will keep doing. This study adds some more guidance. We should accumulate the equivalent of 30 minutes of moderate activity 5 days/week (150 minutes/week) or 15 minutes of more vigorous activity (75 minutes/week). This will reduce our risk of death significantly. But if we engage in muscle training (strength training) a couple times a week we will see the greatest benefit, up to a 40% decrease in mortality! So be sure to add some resistance training to your routines. It will give you the most bang for your time and add the greatest amount of benefit to your life. Remember, something is always better than nothing. Just move!
Additionally, one of the specific cause-specific mortality measures studied was influenza and pneumonia. While this doesn't specifically address COVID-19, it is compelling that this study found exercise reduced deaths due to a viral disease (influenza) and pneumonia. Based on this, increasing our exercise during this pandemic is certainly makes sense.
This chart shows moderate vs vigorous activities
|
|
The Child Is Not to Blame
|
Children are frequently blamed for being excellent transmitters of viral illnesses to adults. They are exposed to lots of other kids in school and childcare settings, they touch everything including surfaces, other kids, their faces and put things in their mouths. Are they high transmitters of COVID-19? This certainly is a huge question as we look for ways to open schools safely. We don't know all the answers, but some studies are suggesting that children may not be great transmitters of this particular virus. In this study out of Switzerland, most children were infected from family members by adults. Only 8% of cases had a child as the index case in the family.
- Since the onset of coronavirus disease (COVID-19) pandemic, children have been less affected than adults in terms of severity and frequency, accounting for <2% of the cases. Unlike with other viral respiratory infections, children do not seem to be a major vector of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission, with most pediatric cases described inside familial clusters and no documentation of child-to-child or child-to-adult transmission. The aim of this work was to describe the clinical presentation of the first 40 pediatric cases of COVID-19 in our city and the dynamics of their familial clusters.
One of our toughest decisions as a country will be how we open or do not open our schools. An editorial accompanying this article has several points which I will outline here. Besides this study, a study out of China early in the pandemic showed 95.5% of children were infected by adults. Another showed only 1 of 10 hospitalized children had transmissions that were thought to be child to adult. In New South Wales, Australia, 9 students and 9 staff infected with SARS-CoV-2 across 15 schools had close contact with a total of 735 students and 128 staff. Only 2 secondary infections were identified, none in adult staff; 1 student in primary school was potentially infected by a staff member, and 1 student in high school was potentially infected via exposure to 2 infected schoolmates.
It seems that spread of COVID-19 is different than influenza and perhaps children will not be the major drivers of the pandemic and perhaps school-based transmissions could be managed. It isn't clear why this is the case and perhaps further experiences will change our vision. I would encourage you to read the entire editorial.
An additional factor is consideration of the effects of modified school on our children and the future of our country.
- A study looking at the effects on children who lived through teacher strikes (avg 88 days of school lost) in Argentina found that 30- to 40-year-olds who lived through the strikes earned 3 percent less than they otherwise would have. This amounted to an annual loss of more than $700 million to the Argentine economy. The children of the students affected by the lost learning time also had lower educational outcomes, implying that a large learning loss may pass down from generation to generation. This seems to be a reasonable equivalent to what our children have experienced.
- A McKinsey & Company report paints a very grim picture regarding achievement gaps for our children, especially those in lower socioeconomic environments.
"Learning loss will probably be the greatest among low-income black, and Hispanic students. Lower-income students are less likely to have access to high-quality remote learning or to a conducive learning environment, such as a quiet space with minimal distractions, devices they do not need to share, high-speed internet, and parental academic supervision."
"The virus is disrupting many of the supports that can help vulnerable kids stay in school: academic engagement and achievement, strong relationships with caring adults, and supportive home environments. In normal circumstances, students who miss more than ten days of school are 36 percent more likely to drop out. In the wake of school closures following natural disasters, such as Hurricane Katrina (2005) and Hurricane Maria (2017), 14 to 20 percent of students never returned to school. We estimate that an additional 2 to 9 percent of high-school students could drop out as a result of the coronavirus and associated school closures-232,000 ninth-to-11th graders (in the mildest scenario) to 1.1 million (in the worst one)."
"
we estimate that the average K-12 student in the United States could lose $61,000 to $82,000 in lifetime earnings (in constant 2020 dollars), or the equivalent of a year of full-time work, solely as a result of COVID-19-related learning losses. These costs are significant-and worse for black and Hispanic Americans. While we estimate that white students would earn $1,348 a year less (a 1.6 percent reduction) over a 40-year working life, the figure is $2,186 a year (a 3.3 percent reduction) for black students and $1,809 (3.0 percent) for Hispanic ones."
"We estimate a GDP loss of $173 billion to $271 billion a year-a 0.8 to 1.3 percent hit."
"The result of this could be the "equivalent of a permanent economic recession"
I certainly don't have all the answers and this is an incredibly uncertain and difficult time. Children can get COVID-19. Thankfully, they seem to generally do well in the vast majority of cases (more so than with influenza). Over 2000 children died during the 2009 H1N1 pandemic. The studies previously published seem to suggest that children are more likely to be asymptomatic or have mild symptoms with COVID-19. We have seen that asymptomatic people tend to spread the virus less than others (not to be confused with presymptomatic
people who are known to spread). This may be the case for children.
I was just getting ready to send this out and I saw an
article come out
from a YMCA overnight camp in Georgia which found that 44% of the staff and campers subsequently tested positive (76% of attendees who were tested were positive). This is a different situation than school since the children were staying in cabins together, didn't wear masks (although the staff reportedly did) and engaged in a lot of singing and shouting as part of the experience. That being said, it certainly complicates our decision as parents, educators, and a society on reopening our schools. It is obvious that nothing can take the place of in person learning and this definitely needs to be our goal. How to achieve this keeps getting more complicated. The stakes are incredibly high for the future of our children and our country.
|
|
Thank you for taking the time to read through this newsletter. I hope you have found this information useful as we work together to optimize your health. Feel free to pass this on to anyone you think would benefit from this information.
You can find previous newsletters archived on my website here.
As always, if you have questions about anything in this newsletter or have topics you would like me to address, please feel free to contact me by
email
, phone, or just stop by!
To Your Good Health,
Mark Niedfeldt, M.D.
|
|
|