
Advancing Public Policies for People with Mental Illness, Chemical Dependency or Developmental Disabilities
|
|
 |
|
|
 |
|
|
First-Ever National Health Plan Survey: Trends In Behavioral Health

Within the report are insights and information related to today's health and human services landscape, including:
- An overview of critical and current national policy shaping the U.S. health and human services and behavioral health markets
- An in-depth review of the unique state behavioral health delivery systems created using a combination of historical practices, federal and state policy, and market factors
- An exploration into health plan practices that are managing the health care and behavioral health care for over 75% of the U.S. population
- An inside look at the consumer perspective of behavioral health regarding access to inpatient services, quality of care, and the performance of the health plans in managing these services
The report and the national survey were conducted in conjunction with Otsuka America Pharmaceutical, Inc. (OAPI), Lundbeck, LLC, and the market intelligence team at OPEN MINDS. In addition, an industry advisory board provided input on the report.
|
|
 |
|
|
 |
|
|
SAMHSA Announces Availability of Up to $23.4 Million for the Infant and Early Childhood Mental Health Grant Program
SAMHSA is accepting applications for the Infant and Early Childhood Mental Health Grant Program totaling up to $23.4 million over the next 5 years. The purpose of this program is to improve outcomes for young children by developing, maintaining, or enhancing infant and early childhood mental health promotion, intervention, and treatment services. SAMHSA expects to fund up to 9 grantees with up to $500,000 per year for up to 5 years. Read more
here.
|
|
 |
|
State Seeks Health Workforce Retraining Proposals
The state Health Department is seeking proposals for health-care workforce retraining programs, with up to $12.9 million earmarked for programs aimed at New York City. Up to $1.9 million will go to projects on Long Island.
In all, the state plans to disburse as much as $18.3 million for the two-year contracts, according to the
request for applications
posted online.
The state seeks proposals that address the need for public health and health-care workers to acquire new skills and to train individuals for new job opportunities resulting from market changes and layoffs. Other program focuses include addressing occupational shortages, developing skills to support emerging technologies, such as telehealth, and meeting the need for data production and analytic skills.
Organizations that may apply for the grants include health worker unions, general hospitals, long-term- care facilities, home health agencies, labor-management committees and educational institutions. The state is particularly interested in proposals that target job categories where there are demonstrated shortages. They include clinical laboratory technologists, registered nurses, licensed practical nurses and nurse practitioners and psychiatric nurse practitioners, physician assistants and home health aides. Applications due by 4 pm June 22.
|
|
 |
|
National Council for Behavioral Health and National Alliance for Recovery Residences
Issue Recovery Housing Toolkit
To help address the nationwide addiction crisis and strengthen the road to recovery, states need to invest in access to quality recovery housing. Evidence shows that recovery housing is instrumental in helping individuals with substance use disorders achieve and sustain a life in recovery. Despite this, recovery homes are often under-resourced and excluded from public sector policies and resources. In response, the National Council for Behavioral Health and National Alliance for Recovery Residences (NARR) issued
Building Recovery: State Policy Guide for Supporting Recovery Housing to assist states with the creation of recovery housing certification programs that standardize recovery housing operations to protect and support residents.
Building Recovery provides states the knowledge and guidance to adopt recovery housing standards, incentivize compliance and invest in recovery housing infrastructure. The toolkit also includes sample resources such as a model state law, a legislative matrix of current and proposed recovery housing bills, an action assessment and list of research briefs that are publicly available for review.
|
|
 |
|
|
May 15, 12 - 1 pm, SAMHSA
Exploring the Impact of Trauma on Parenting
May 15, 12 - 1 pm, CTAC
How Community-Based Behavioral Health Treatment Providers Can Develop and Implement Collaborative Comprehensive Case Plans
May 15, 2 - 3:30 pm, National Reentry Resource Center
Person-Centered and Collaborative: New Safety Assessment for Suicide Prevention
May 16, 1 - 2 pm, National Council for Behavioral Health
Avoiding Burnout: Learning To Live & Work Well In Health Care
May 17, 12 - 1 pm, PsychU
Evaluation of Data Collection with Rochester Regional Health
May 18, 12 - 1 pm, CTAC
Addressing Behavioral Health Needs of Older Veterans: In our Communities and in Partnership
May 22, 12 - 1 pm, SAMHSA
Social Media/Technology for Outreach and Engagement
May 23, 1 - 2 pm, SAMHSA
The Roles of Behavioral Health in Early Diversion
May 24, 2 - 3:30 pm, SAMHSA
Redefining Care Management in Medicaid Managed Care
May 24, 3 - 4 pm, Manatt Health
Getting to the Heart of Motivational Interviewing
May 30, 12 - 1 pm, CTAC
How Media & Movies Shape Our Perception Of Serious Mental Illness
May 31, 12 - 1 pm, PsychU
The Interplay Between Sleep & Bipolar Disorder
June 5, 12 - 1 pm, PsychU
Mental Health Apps on your Smartphone: Do they work?
June 5, 12 - 1 pm, SAMHSA
June 6, 12 - 1 pm, SAMHSA
Understanding the complex lives and needs of people with co-occurring mental illness and I/DD
June 12, 12 - 1 pm, SAMHSA
June 12, 3 - 4 pm, Manatt Health
|
|
 |
|

|
CALENDAR OF EVENTS
MAY 2018
Children & Families Committee Meeting
May 15: 11:30 am - 1 pm, GTM
Mental Hygiene Planning Committee Meeting
May 15: 1 - 3 pm, GTM
Developmental Disabilities Committee Meeting
May 17: 1 - 2:30 pm, GTM
Agency Meeting: NYS OASAS
May 23: 10 am - 12 pm
1450 Western Ave., Albany
Agency Meeting: NYS OMH
May 23: 1 - 3 pm
44 Holland Ave., Albany
Office Closed: Memorial Day
May 28
JUNE 2018
Officers, Chairs & Regional Reps Call
June 6: 8 am
Mental Hygiene Planning Committee Meeting
June 18: 1 - 3 pm, GTM
Children & Families Committee Meeting
June 19: 11:30 am - 1 pm, GTM
Directors/Executive Committee Meeting
June 20: 9:30 am - 12:30 pm, GTM
Contact CLMHD for all Call In and Go To Meeting information, 518.462.9422
|
|
|
|
New York City Moves to Create Safe Injection Sites
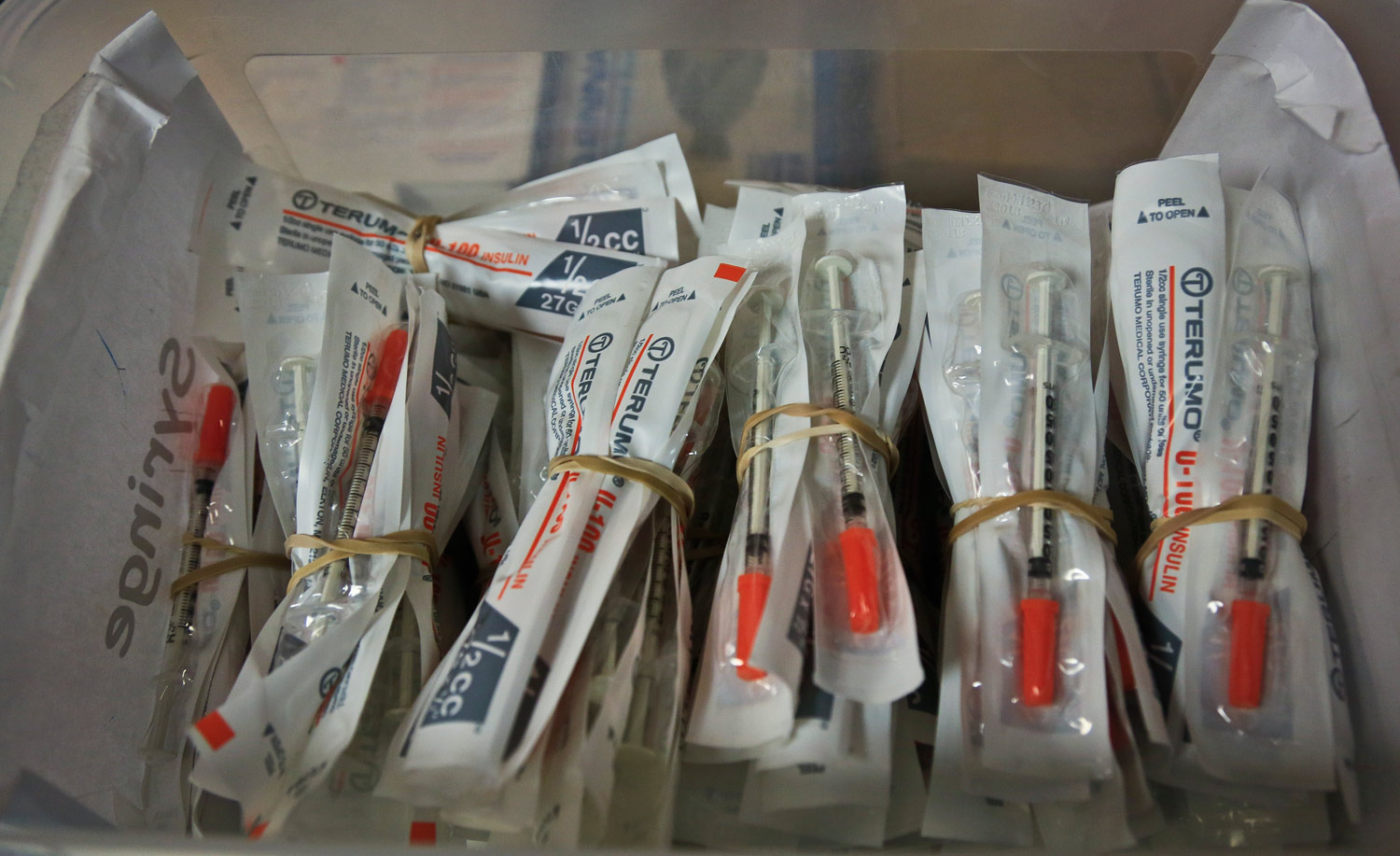
Mayor Bill de Blasio is championing a plan that would make New York City a pioneer in creating supervised injection sites for illegal drug users, part of a novel but contentious strategy to combat the epidemic of fatal overdoses caused by the use of heroin and other opioids.
Safe injection sites have been considered successful in cities in Canada and Europe, but do not yet exist in the United States. Leaders in San Francisco, Philadelphia and Seattle have declared their intention to create supervised sites, although none have yet done so because of daunting obstacles. Among them: The sites would seem to violate federal law.
The endorsement of the strategy by New York, the largest city in the country, which last year saw 1,441 overdose deaths, may give the movement behind it impetus.
For the sites to open, New York City must still clear some significant hurdles. At minimum, the plan calls for the support of several district attorneys, and, more critically, the State Department of Health, which answers to Gov. Andrew M. Cuomo. The city sent a letter on Thursday to the state, asserting its intention to open four injection centers.
View full story from
The New York Times.
|
|
 |
|
|
New Approach to Drug Crime Gains National Attention
In the fourth of a series on opioids, the Times Union focuses on how one police department decided "We can't arrest our way out of this."
When Rudy Fernandez found heroin he found love.
He was 18 or 19, he remembers, and he had tried other recreational drugs. But marijuana and cocaine never made him feel like this, like he was OK and the world was OK and not only was it OK, it was great, even if his mom loved drugs more than him and the Dominican-born boy had never felt at home in this English-speaking place.
"It took away everything I'd been searching for my whole life, because it was love, literally love," Fernandez, recalled, more than two decades later. "I'd be a liar if I told you I didn't love that. It made me feel whole because I didn't know no better."
Raised by a drug-addled mother in the Bronx, Fernandez quickly learned that drugs were love and the streets were home. And because he committed crimes to maintain that way of life, he spent the next 22 years cycling in and out of correctional facilities, where drugs were readily available to continue his habit.
It wasn't until 2014, when Fernandez was tired and his parole officer was tired that they decided to try something new. The officer referred Fernandez to Hope House, a residential addiction recovery program in Albany. Read more
here.
|
|
 |
|
|
One State's Opioid Success Story
In recent years, most states have devoted increased resources to easing the transition of prisoners back into society through job training programs and, in some cases, therapy and counseling. But few provide effective drug treatment programs, such as methadone maintenance. Given the rising number of opioid deaths, they might want to consider doing so.
The period immediately after release from prison is a dangerous time for addicts. They've experienced a stretch of enforced, if not total, sobriety. Suddenly they have access to drugs, but their tolerance level has diminished. The stress of re-entry and the difficulty finding jobs and housing don't help. One study of released prisoners in Washington state found that they were 13 times more likely to die from drug overdoses than the population as a whole.
In Rhode Island, the Corrections Department now provides medical addiction treatments to criminals while they are still incarcerated. The results have been striking. Between 2016 and 2017, the number of deaths among recent ex-prisoners dropped by 61%. That was enough to bring down the total number of overdose deaths in the state as a whole by 12%, even at a time when opioids are driving up the death rate in most places. Read more
here.
|
|
 |
|
The Struggle Of Finding Help For 'A Dangerous Son'

A new
HBO documentary tells a story about families with children who have psychiatric disorders that lead to violent behavior.
A Dangerous Son focuses on three families who are dealing with the simultaneous challenges of handling children prone to lashing out while looking for treatment that is not always available.
"I don't know how to control my anger," 10-year-old Ethan says in one clip.
Ethan, now 16, is one of the film's subjects. His mother Stacy Shapiro says he struggles with autism, attention deficit hyperactivity disorder, oppositional defiant disorder, intermittent explosive disorder and anxiety. His aggressive behavior started between ages 2 and 3, she says.
He lashes out frequently over small things - a scene in the movie of him hitting and shouting in the car is "a daily occurrence for us, sometimes multiple times a day," Shapiro tells NPR's Lulu Garcia-Navarro on Weekend Edition.
They sent Ethan to a residential mental health facility, which is documented in the film. That's not an option for many families, as there aren't enough beds in many areas. Read more
here.
|
|
 |
|
|
NYS Empire State Supportive Housing Initiative (ESSHI) RFP
On May 1, 2018, NYS released its third-round Empire State Supportive Housing Initiative (ESSHI) Request for Proposals (RFP). The State intends to develop a total of 20,000 units over the next 15 years. As such, the State is issuing this RFP to advance the five-year goal of developing more than 6,000 units of supportive housing over five years. Funding for at least 1,200 qualifying individuals will be awarded through this third-round RFP.
The eligible target populations to be served under this program are families with a qualifying individual, individuals and/or young adults who are both homeless and who are identified as having an unmet housing need as determined by the CoC or local planning entity or through other supplemental local, state and federal data, AND have one or more disabling conditions or other life challenges.
NYS Office of Mental Health (OMH) is the lead procurement agency for this RFP. New York State will award up to $25,000 in services and operating funding per qualifying individual annually. Other State agencies may administer contracts for populations not overseen by OMH.
Changes have been made to the Frail Elderly population definition and the Medicaid Redesign Team (MRT) requirements from last year's RFP.
To view the RFP on the OMH website, click
here.
|
|
 |
|
|
ACTION REQUESTED: Message from the NYS Commissioner of Health and the Acting Director of the NYS Office for the Aging
In Governor Cuomo's 2018 State of the State, he announced the launch of a Long Term Care Plann!ng Council to prepare for the emerging needs of New York State's growing aging population.
The charge of the Council is to examine New York's long term care system. The NYS Department of Health and the NYS Office for the Aging are requesting that you complete a brief anonymous survey to assist the Planning Council in this effort. For the purpose of this Council, the "long term care system" should be broadly interpreted to include a variety of services and supports that help meet both the medical and non-medical needs of individuals with a chronic illness, disability, or functional need, and includes services and supports for caregivers. The results from this survey will be used in the deliberations of the Long Term Care Planning Council.
To access the survey, click
HERE. Please respond by June 18, 2018.
|
|
 |
|
CMS Announces Agency's First Rural Health Strategy

The Centers for Medicare & Medicaid Services (CMS) this week released the agency's first Rural Health Strategy, which is intended to provide a proactive approach on healthcare issues to ensure that the nearly one in five individuals who live in rural America have access to high quality, affordable healthcare.
The agency-wide Rural Health Strategy, built on input from rural providers and beneficiaries, focuses on five objectives to achieve the agency's vision for rural health:
- Apply a rural lens to CMS programs and policies
- Improve access to care through provider engagement and support
- Advance telehealth and telemedicine
- Empower patients in rural communities to make decisions about their healthcare
- Leverage partnerships to achieve the goals of the CMS Rural Health Strategy
Approximately 60 million people live in rural areas - including millions of Medicare and Medicaid beneficiaries. CMS recognizes the many obstacles that rural Americans face, including living in communities with disproportionally higher poverty rates, having more chronic conditions, being uninsured or underinsured, as well as experiencing a fragmented healthcare delivery system with an overworked and shrinking health workforce, and lacking access to specialty services.
This new strategy focuses on ways in which the agency can better serve individuals in rural areas and avoid unintended consequences of policy and program implementation.
For more information on the Rural Health Strategy, click here.
|
|
 |
|
Telehealth Use in Behavioral Health Cases Shows Promise in Cost Control, with Utilization on the Rise
Telemedicine technology has been improving steadily over the past several years, and as the tech gets better, so does its reputation.
Increasingly, payers and providers are realizing that telemedicine has the potential to control costs, but the sector has now crossed a threshold. Complex clinical cases and behavioral health are now being treated viably using a virtual approach.
Much of telemedicine's appeal lies in accessibility. The lack of access to care through telemedicine negatively affects
patient engagement and follow-through, according to new research from telehealth provider Teladoc. Treating mental health in particular becomes easier, less costly and less stigmatized when behavioral health treatment can take place in a virtual setting.
"Increasingly, people who are suffering from behavioral health disorders are recognizing that virtual care can often be a highly effective solution," said Dr. Lew Levy, Teladoc's chief medical officer. "About 42 million Americans have anxiety disorders, and more than 16 million suffer from major depression. But most haven't received treatment in the prior year."
That's problematic, because in the U.S., 70 percent of people with a behavioral health issue also have a medical comorbidity, the research showed. Read more
here.
|
|
 |
|
What's Holding Up Community-Based I/DD Services?

The push to move consumers needing long-term services and supports (LTSS) out of residential placements and into community settings continues. Part of the push is that there are currently 59 lawsuits related to Olmstead open across the country, which require states to find ways to support care individuals in the community. And there are the cost issues. The majority of the services-both institutional and community-based-required to support these consumers are covered by Medicaid. Generally, the community-based options are less expensive than residential care options. But while there are an estimated 6.2 million people with I/DD who are on the Medicaid roles, only 689,144 (11.2%) are receiving HCBS services. An estimated 200,000 are on state HCBS waiver waiting list for those services.
The raises the question, what's the hold up? A recent congressional briefing identified four major challenges to HCBS availability for consumers with I/DD. These challenges include lack of state funding causing waiting lists, high staff turnover rates and overall lack of adequate numbers of direct support professionals, state reliance on unevenly skilled family caregivers, and limited housing opportunities. Without addressing these issues, the numbers of consumer with I/DD with the option of living in the community will continue to lag.
Waiting Lists & State Funding Shortages--
Nationwide, about 75% of Medicaid funding for LTSS is for HCBS for people with I/DD. Community-based services are less expensive than the 24/7 care of a residential setting - the annual cost of care for a consumer receiving HCBS supports is about 13% less than residing in a state institution, and about 20% less than residing in an intermediate care facility (ICFs). If HCBS save state Medicaid programs money, why are there still wait lists? Because HCBS are an optional, waiver-based Medicaid service. This means that as states are balancing their budgets, other mandatory programs and services included in Medicaid state plans must be funded first
. Medicaid HCBS funding would need to increase by 26% nationally to account for state budget shortfalls that would allow funding for all consumers on wait lists. Read more here.
|
|
|