|
New Bay Cove Crisis Line Phone #
As of July 1, 2018, the 24-hr Bay Cove Crisis Line will be changed to:
833 BAY-COVE (229-2683)
|
|
|
 |
|
From the desk of Jackie Lane, Executive Director NAMI CC&I

In defense of families!
Conventional wisdom says that those with mental illness have a better chance as they go into recovery if they have a loving and supportive family. Over the past few weeks we have had a marked increase in support calls from parents of adult children who are in need of help and support as they try to get services for their children. It is interesting that in the cases of which I, personally, am familiar, the adult children are all male and range in age from the mid-twenties to the mid- forties. Those in the mid- forties have had mental health issues for several years, and it has been a constant struggle for concerned parents and families. In my own personal life, I have witnessed these same issues and frustrations endured by my parents as they dealt with my brother from the time he was diagnosed at age twenty until their deaths many decades later. This personal history, as well as observing and helping with the problems faced by these five families over the past few days, has renewed my desire to explore and hopefully better understand the issues which arise for families trying to help adult children during a mental health crisis.
There are three issues which come to mind as the most frustrating for those trying to help. Two of these issues, the HIPAA laws and the Section 12 guidelines, are rooted in legalities and are confusing and are often interpreted in different ways. The third issue is the very role of families as seen by the staff that cares for the mentally ill person.
The HIPAA laws, enacted to ensure the privacy of medical records, are often very frustrating when applied to a mental health crisis. In theory, if the patient is of age, they prevent any medical information from being shared with family members. They will often prevent the family from even learning if their loved one has been admitted to a facility. Privacy is very important, and due to the remaining stigma about mental illness, people often feel the need to keep any treatment for mental health especially private. A medical facility can share information with a family if the patient signs a release form granting permission. However, in reality, when a person is undergoing a mental health crisis, this is very often the very last thing that they are going to do. You are actually asking a person who is not thinking clearly in his present state to make a rational decision. So very often, the family is cut out of the whole process and suffers extreme anxiety not knowing about treatments, diagnoses, or prognoses. One thing for the family member to remember is that even though the medical worker cannot disclose information to them, they can talk to the medical staff and relay important information to them. I would hope that a good doctor or nurse or social worker would listen and get all the background information possible. These parents have been living with this situation and can very well have more insight than even a very good doctor or other staff member can gain in a short observation time.
Section 12, is a legal device used to admit a person to treatment without their consent. It is most often used by the police when they witness a person in a severe mental crisis who is unwilling to go for help or refuses to admit that he needs help. The standard phrase used to determine if a person should be sectioned "is he an imminent danger to himself or others." Again, this can be subject to interpretation. One interpretation is "is this person at this very time suicidal or homicidal?" There have been some new federal guidelines of late and they are worth examining. In the past week, I have seen a person with a long history of mental illness and hospitalizations being seen as 'unsectionable' and then finally sectioned and released by a hospital. He was finally re-sectioned and held a few hours later after decompensating further. Again, the family who knows the history of the individual could have predicted this. I have been told, and I saw it in my brother, that each time a person decompensates and as he ages, it is doubtful that he will regain his former baseline. I know that the law is protecting the person's freedom, but again, if a person is in a mental health crisis, is he capable of deciding if he needs medical treatment. Family members who have been involved with the individual can often determine danger points based on experience and history.
And finally, it appears that families are sometimes not treated respectfully by medical workers. They are seen as part of the problem rather than as a part of the solution. The families with whom we interact have often taken our Family-to-Family course, attend support groups, and seek information and education regarding their loved one's conditions. Having a mentally ill child changes one's life from the norm to a life of walking on eggshells and waiting for the other foot to drop. Again, I repeat, conventional wisdom says that those who have a supportive family have a better chance of staying in recovery. Between HIPAA laws, very high thresholds for sectioning, and lack of collaboration with medical staff, the caring family suffers. We will continue to do all we can to support the families that come to us when there is a mental health crisis with a loved one.
|
|
 |
 |
 |
 |
 |
 |
NAMI CAPE & ISLANDS EDUCATION PROGRAMS
An important aspect in recovery of any illness is the care and support one receives during the healing process. Education, awareness, and empathy on behalf of any caregiver, family member or friend who is in that role can be instrumental in the success and outcome of a recovery.
At NAMI Cape & Islands we strive to provide quality support and education to people who find themselves in the position of caring and advocating for someone coping with a mental health challenge.
Through education, people learn to meet the challenges that are often present when advocating for someone in need of mental health care. With support, people find the strength and resilience to manage those challenges. The outcome of education and support enables people to stay healthy themselves during a difficult journey as well as improve the recovery outcome for the individual battling their illness.
Family-to-Family
is a program for family and friends of people with a mental health challenge. The course that meets weekly for 12 weeks teaches people about the various mental health conditions, medications commonly used, communication skills, self-care, and problem management.
Classes ongoing in Barnstable and Falmouth.
New sessions to begin on Nantucket and in Wellfleet - Winter 2019
Family Connections
is a course developed by the National Education Alliance for Borderline Personality Disorder. This course is helpful for people who love someone who has difficulty with emotional regulation. This course meets weekly for 12 weeks and helps people to learn about this disorder, how to better communicate and promote healthy relationships, as well as develop empathy for the emotional pain that is present.
Next course to begin in the Spring 2019 - Barnstable
For the Brazilian Community:
Sau'de Mental Um Deito De Todos (Mental Health Awareness)
Quando a familia chega perto a droga fica longe (Prevention, Education and Intervention Guide for Parents and Caregivers regarding the effects of Alcohol, Drugs and Mental Health in Youth)
Os Impactos De um Diagnotico Mental (Mental Health Diagnosis Course) - To begin on October 15, 2018 - Hyannis
Mental Health First Aid:
NAMI Cape & Islands recently trained 13 Mental Health First Aid instructors on Cape Cod. Mental Health First Aid instructors are able to facilitate an eight-hour program to educate people to become mental health first aiders. It is like CPR for mental health. - Next session at Centerville Library - October 22 & 23
Homefront is a six-week course similar to Family to Family for military families. This is a new program to Massachusetts, and currently will only be available on Cape Cod.
To get information or register for any of NAMI Cape & Island education and support programs, contact Kim Lemmon, Director of Family Programs, at 508-778-4277, or email [email protected]
|
|
 |
Resiliency: Bouncing Back from Relapse
Recovery is not about never getting sick again-it's about bouncing back when you do.
I
often feel as if I've stepped back in time when I get really sick. I think, "How could this happen again? I've worked so hard to get where I am!" Just a few weeks ago, I made this comment to my therapist after I had trouble at work and went into a
depression
. She replied, "Julie, you always tell me to remind you that it's an illness. You have bipolar disorder, so getting depressed after a stressful event is what happens. You do get sick, but it's not like it used to be. What's different is your resilience-you're able to bounce back a lot more quickly."
She's right. In the past, if I got depressed it would last for a year. Progressively, I got it down to six months, a few months, and finally just a few weeks. In fact,
relationship problems that used to send me into a depressed, sometimes psychotic, tailspin may now only take a weekend to resolve.
Indeed, I can bounce back instead of breaking apart like I used to. I kept working on my bipolar management skills until I turned myself into a rubber band that stretches in and out of any situation. That is how I describe resilience: When we are resilient we can handle any of the problems that come with bipolar. This is because we can "stretch" ourselves to meet any circumstance, even when we are really ill.
What about triggers?
I've tried to remove the
triggers in my life that I know will make me ill, and have written about this effort before. But I can't control everything. In the past, I wasn't very smart about bipolar. I would get myself into situations that were clear triggers in the past, get sick in the same way, and then wonder why. In other words, I believed I could walk into fire and not get burned by bipolar disorder. I now realize that resilience doesn't mean you make the same mistakes, hoping you can deal with them more effectively. Rather, resilience comes from stopping certain behaviors that make one sick, then using the resulting energy to manage daily life instead of being in a constant crisis mode.
The resilience pendulum
Bipolar disorder mimics a pendulum that swings way out to each side before it returns to the middle. The swings on the edges are about suicidal thoughts, humiliation, dangerous manic choices, letting the wrong people into your life, and not accepting the limitations of bipolar. Luckily, as you change your behavior-even just a little bit-the pendulum stays closer to the middle. Eventually, it will only swing out to the edges when something occurs that's beyond your control. This is true
resilience and it feels good!
Tips for becoming more resilient
Look at yourself before accusing others of upsetting you: Sure, they may be totally to blame, but you and your bipolar disorder treatment come first. Ask yourself, "What about this situation might be triggering behavior characteristic of bipolar?" "What do I need to do right this minute to take care of myself?" Then you can talk to the other person and explain how his or her behavior or insensitive words may have triggered a
mood swing. Such an approach will help you bounce back. This is because you haven't added a confrontation, or an accusation, on top of your already stressed brain.
Watch out for behaviors and situations that affect sleep. People who have bipolar disorder are notorious for sleep problems. For us, hormones such as serotonin and melatonin can be completely messed up by many things, including weather, worry, or the illness itself. Resiliency requires restful sleep-this fact can't be stressed enough. So even if you're sick and worried and feel you can't go on, you need to regulate your sleep. This means staying out of bed during the day and getting to bed at the same time each night. Sure, it's hard and sometimes it's impossible, but you still must try. This is one of my biggest difficulties-sometimes I can't sleep at all when I'm
hypomanic. Yet I realize that I must find a way to sleep, if I am to deal with life's pressures.
Teach the people in your life how to help you when you have a setback. Tell them exactly what they can do. "Mom, when I have a terrible day at work and feel completely
paranoid, please point it out. You can say, 'Julie, you talk like this when work is stressful. You asked that I remind you that it's the bipolar and not really you. You asked for my help and told me you don't want to ruin things like you did at your last job.'" I kept working...until I turned myself into a rubber band that stretches in and out of any situation.
Adhering to this strategy can help one bounce back from a potentially dangerous situation. This way, too, you can go to work the next day and get on with your job. That is resilience!
These are just a few examples of how making some healthy changes can help you remain strong and supple like a branch that bends without breaking. Sorry for all the metaphors, but they really are appropriate here. Think of yourself as a wave, or a child who falls down and gets back up. Resiliency really is all about flexibility. If you think about it, bipolar disorder is black or white: It's mania and depression-elation and desperation.
And it makes us view the situations themselves as black-and-white. This was terrible. I'm going to die. I won't make it through this. It doesn't have to be this way, however.
A new you
What would it be like if you were as flexible as the strong rubber band I've been describing? What would it feel like to know you will be okay? I find it comforting to know that I can-and will-handle things. I now can be strong when I'm showing symptoms. Even if someone I love dies, I know I have the tools to survive. I may have to be in the hospital to do this; I may be suicidal or go into a
manic episode. Yet each day I have gradually increased my ability to handle a crisis since my diagnosis 23 years ago.
It definitely takes the help of everyone I know, including my doctors and my therapist. I have also taught people how to help me be resilient. All of us, whether or not we have bipolar, must spend a lifetime improving our ability to bounce back from anything life throws at us. The more we do this, the more resilient we can become.
Written February 16, 2010
|
|
 |

|
 |
 |
Book Review
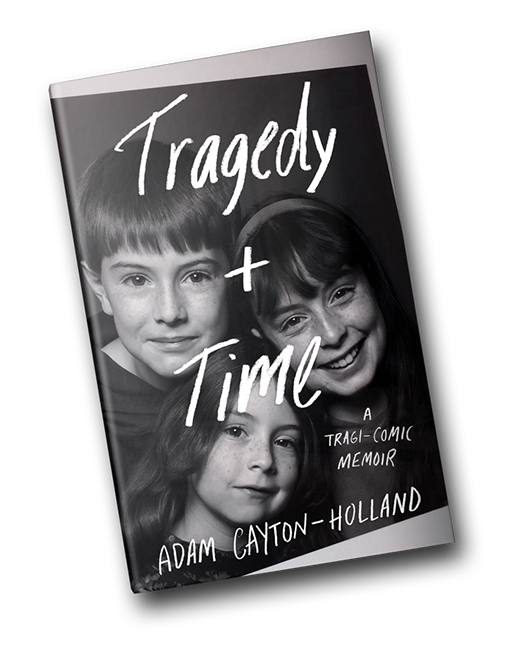
Tragedy & Time: A Tragi-Comic Memoir
by
Adam Cayton-Holland
Adam Cayton-Holland is a comedian and writer who has written a book about the tragic suicide of his beloved younger sister and its impact on himself and his family. This book is powerful, sad and straight from the heart. It is a loving description of the life of a closely-knit family that is shocked and devastated by the death of their youngest child.
The first part of the book focuses on the author's developing career as a stand-up comic and growing up in a family of five in Denver. He describes his younger sister, Lydia, as a smart, sensitive and empathic person. "For most of her life, she glowed. She was this awesome original; this strange, funny, powerful force."
He then writes about his own emotional difficulties in college and then of Lydia's gradually increasing difficulties in young adulthood leading to emotional breakdowns. He talks about the difficulty everyone in the family had trying to understand what was happening. It was equally difficult for mental health providers to reach a clear diagnosis and treatment program. What was clear in retrospect was the suffering that she faced.
When family members received a brief email from Lydia saying "Love you all.", they knew something was wrong. Adam went to her home only to discover that she had committed suicide. The author and his family were devastated. Adam Cayton-Holland writes about the ensuing grief and pain that he felt. He talks about the unpredictable explosions of grief. He talks about the suffering of his family. He finds benefit from EMDR (Eye Movement Desensitization and Reprocessing) to deal with the trauma of finding his sister. He also finds solace in meeting a friend of a friend who also lost a sibling to suicide.
In writing about his experience both online and in this book Cayton-Holland has reached out to many people who have either suffered through a loved one's suicide or fear that it may happen. This book is important for two reasons. I believe that it has helped the author's own healing and hopefully readers, themselves, may find it a help as well.
Written by Dr. George Vitek, retired pediatrician who practiced for 28 years in Wilbraham, MA. Married father of four and grandfather of 9.
|
|
 |
 |
 |
 |
 |

 |
|
 |
Suzanne Fronzuto
NAMI on Nantucket Program Coordinator
|
I recently attended a conference on Housing and People with Serious Mental Illness and the message from every speaker was; "you can't stabilize without housing". Attendees were challenged to remember that every number, every diagnosis is a human being. Housing alone is not the solution, however. Without on-going community supports to give a voice to those without a rental history and part-time work experience, the building relationships part of recovery will not happen. This made me think about the housing situation in Nantucket where there has been talk over the years of buying or building condo units to house those in recovery, a process that may take more than a year. Does Nantucket currently have adequate community supports? Sadly, the response is similar to that of many other communities; "we're not there yet".
Senate President, the Honorable Karen E. Spilka gave the opening address and delivered the message that "it must be a state priority to reduce the stigma" associated with mental health and Gov. Charles Baker in the 2019 Massachusetts state budget has made secure housing a priority by increasing the allocation for rental subsidies for DMH clients and earmarking additional millions for mental health and intellectual disability housing. Senate President Spilka went on to say that we need to do more and solutions won't come from the legislature but those doing the work.
It was eye-opening to hear from agencies that find and supervise housing opportunities in communities throughout Massachusetts. While having family supports are an important part of recovery, clients may have to leave familiar surroundings and relocate to a town with limited access to public transportation, away from family- simply because that's where the open bed is.
There are people ready and waiting; to leave the hospital, to leave group homes, to leave home. Some have been waiting longer than 2 years, and they are stuck like quicksand in their present situation due to lack of housing. The Massachusetts Olmstead Plan 2018 which can be read online was recently released with 41 pages of highlighted progress and future goals to expand community based supports including permanent, supportive housing solutions in the Commonwealth of Massachusetts.
The final take-away from the conference was "there is always hope". For those of us affiliated with NAMI as volunteers, advocates, service providers or consumers we carry that torch of hope with us always as we strive to move beyond "we're not there yet".
|
|
 |
|
NAMI on the Vineyard


September was a busy month for NAMI on MV. We held our first ever fundraiser on September 14, as a kick off to introduce NAMI to the community. We also formally thanked Fenton and Peggy Burke for their many years of dedicated service to NAMI on MV. Without them we couldn't have educated over 170 people in our family to family classes and supported so many family members in our support groups.
The evening was a great success with close to 100 people in attendance. The live and silent auction donations were a big hit!
A special thank you to Kristie Mayhew and Tammy Silva for their vision and hard work in making the event possible.
We also set up an info table at the International Overdose Awareness vigil which was well attended, and will have an info table at a Suicide Prevention Walk on September 29.
We are hoping to have some teachers from MV attend Think Kids on October 5 at Mashpee HS and some First Responders attend the CCIT session at end of November.
 |
|
 |
Lisa Belcastro
Coordinator
|
Cecilia Brennan
|
|
|
 |
 |

|
Beyond 'Grading the States'
On Monday, the Treatment Advocacy Center released its newest report,
Grading the States: An Analysis of Involuntary Treatment Laws. The report represents the culmination of a year-long project by Treatment Advocacy Center staff to evaluate the unique involuntary treatment laws in all 50 states and the District of Columbia. Each state's laws were analyzed and evaluated for whether the statute promotes the ability for individuals with severe mental illness in need of an evaluation or treatment to do so in a timely and effective manner.
One-third of states received a grade of B or better, with only seven states receiving an A grade. One out of every five states received a failing grade. Of note, it was beyond the scope of the report to analyze how the states utilize the laws, therefore a passing grade does not necessarily mean that the state provides adequate treatment services for individuals with severe mental illness.
Perhaps more important than the evaluation and grade themselves, this report is the first-of-its-kind in laying out the Treatment Advocacy Center's evidence-based policy recommendations. In Section Two of the report, we highlight state laws that allow timely and effective treatment as well as those that impose artificial treatment barriers. Each policy recommendation is bolstered with peer-reviewed research or evidence to support the claim.
Requiring imminent dangerousness
For example, the fifth policy recommendation in the report states the following:
Statutory language defining the "danger to self or others" standard should not require imminence of harm.
Seven states require that harm to self or others must be imminent for qualifying for inpatient commitment, despite the bountiful evidence showing that this severely limits one's ability to receive timely treatment and has long-term consequences on an individual's disease progression. Research shows that statutes that require the individual present an imminent danger to self or others before any intervention leads to criminalization. In a 2008 Journal of Medical Ethics article Dr. Large and colleagues from St. Vincent's hospital in Australia write, "dangerousness criteria unfairly discriminate against the mentally ill, as they represent an unreasonable barrier to treatment without consent, and they spread the burden of risk that any mentally ill person might become violent across large numbers of mentally ill people who will never become violent."
By requiring an individual to decompensate to the point of current dangerousness, the situation is almost guaranteed to become a public safety risk. Law enforcement is trained to handle threats to public safety within the confines of the criminal justice system, leading to the horrible outcomes we have reported on previously, such as having a 16 times higher risk of becoming a fatal police encounter or the overrepresentation of serious mental illness in jails and prisons.
Laws that include only an immediate dangerousness criterion have been shown to lead to longer duration of untreated psychosis, which in turn leads to worsening permanent brain damage. One study reports that individuals who live in countries that utilize a dangerousness criterion for commitment have an average of five months longer duration of untreated psychosis than those who live in countries without a dangerousness criterion. And research shows that the longer an individual has untreated psychosis, the longer it will take to emerge from it, and the less likely the person is to make a full recovery. Timely treatment, before significant decompensation occurs, has been proven to improve an individual's prognosis for the illness course.
For the full list of evidence-based policy recommendations about state involuntary treatment standards, please refer to the full report.
|
|
|
Elizabeth Sinclair
Director of Research
Treatment Advocacy Center
|
|
|
 |
 |
 |
|
EXTREME RISK FIREARMS RESOURCE GUIDE
|
|
|
Governor Charles D. Baker recently signed into law a measure that permits a family or household member who believes that a person who holds a license to carry firearms or a firearms identification card poses a risk or bodily harm to themselves or others, to file a petition seeking an "extreme risk protective order." Such an order would require the individual to surrender their license or Firearms ID (FID) card and any firearms they may possess.
The new law also requires the Department of Mental Health (DMH) to compile a resource guide of mental health and substance misuse services, along with other information, to be provided by the Trial Court to any person who files such a petition or against whom a protective order is issued. DMH developed the required resource guide which contains many links to useful information.
|
|
|
|
 |
 |
 |
 |
 |
 |
 |
 |
Dance In The Rain
Dance in the Rain Peer to Peer Mental Health Center
"Where Healing Begins"
Dance in the Rain is looking for donations of art materials for our open art studio. Canvases, acrylic paints, brushes, drawing paper, frames, and collage materials.
Dance in the Rain Peer to Peer Mental Health Center is open Monday through Thursday 10:00AM to 4:00PM. "Dance..." offers a variety of daily workshops and meetings. We are drop-in style and all of our services are free of charge. Come check us out and experience the healing power of peer engagement.
For more information, contact:
Founder/Executive Director/Peer
Dance in the Rain Whole Person Approach
Peer to Peer Mental Health Center
501 c 3 Non Profit Public Charity
508-364-4045
|
|
 |
 |
 |
|
Transportation Services....
The Cape Cod Regional Transit Authority provides a daily general public demand service called Dial-A-Ride Transportation (DART) that is a door-to-door ride by appointment transportation service. It is available to all 15 Cape towns, runs from 7:00 am to 7:00 pm on weekdays and more limited hours on weekends. It is easy to access and use.
|
|
 |
|
The Primer on Mental Health

WE'RE PUBLISHED!! You Are Not Alone: A Primer on Mental Illness, which has been in development for the past 18 months, is now available. (Call or email the office to make arrangements for your personal copy or copies for your organization.) The Primer has been hugely popular--we published 2,000 copies
and have only 100 left!
The Primer is also online on our NAMI CC&I web site. The production and publication of this 88-page booklet was made possible by generous support from the Cape Cod Healthcare Community Benefits Fund, The Kelley Foundation, Inc. and The Cape Cod Five Foundation.
|
|
 |
 |
 |
 |
 |
|
Tidbits...
For NAMI members:
|
|
|
If you can't go to the convention, please complete an absentee ballot for open NAMI MA Board of Directors seats and vote for
Arlene Goldberg Hoxie so that we can have representation from Cape Cod & The Islands
|
***************************************************
Active Parenting of Teens
The Family Resource Center is offering a 6-week parenting course
Begins Wednesday, October 3 | 5:00-7:00 PM
Dinner & Childcare provided
For more info or to register, call 508-815-5074 or email
*************************
|
Families for Depression Awareness Presents Free Teen Depression Webinar
|
|
|
Thursday, October 11 at 7:00 PM
Presenter Amy Saltzman, M.D. will discuss how caring adults can encourage teens to manage stress. The program is designed for parents, caregivers, school educators and personnel, youth workers, and anyone interested in teen mental health.
Register
here
to join us for a live webinar discussion.
|
******************************************
GRANDPARENTS RAISING GRANDCHILDREN
Grandparents Raising Grandchildren: Legal Advice
Grandparents with questions about guardianship/options can visit the Probate Court on the
3rd Thursday
of the month between 8:30 AM-1:00 PM.
They can also call the Bar Association (508-362-2121) or Susan at the courthouse (508-375-6730) for an appointment with Kathleen Snow on
Mondays
between 10:00 AM-1:00 PM.
There is no fee for either of these consultations.
Lawyer For A Day--Free Legal Advice
Held daily at the Barnstable Probate Court. It is advisable to arrive promptly when it opens at 9:00 am as it is first come, first served and fills up quickly.
I
nclusions in the Newsletter
We have recently been asked for last minute inclusions of events in our newsletter. We have instituted a new policy: It is at the discretion of the Executive Director to determine whether content being submitted for distribution to the membership is aligned with our mission. If the content is determined to be appropriate, it may be included in the monthly e-newsletter if it is submitted prior to the first of the month.
|
| |
|
 |
When shopping on Amazon, think NAMI CC&I and Amazon Smile.
Every dollar you give to NAMI CC&I goes to help support, educate and advocate for the residents of Cape Cod, Nantucket and Martha's Vineyard.
AmazonSmile is a simple way to give when you are shopping on Amazon
Amazon donates 0.5% of your eligible purchases.
It's so easy, you can still use your Amazon Prime and you still collect points. All you need to do is: When you are going to make a purchase on Amazon, first enter
in your internet browser. On your first visit to AmazonSmile, you will be prompted to select a charitable organization .
Select NAMI Cape Cod Inc.
|
|
|
|
|
|
Copyright © 20XX. All Rights Reserved.
|
|
|
|